Preoperative Assessment:
The preoperative history can be organized using a systems-based approach. Pertinent positives should elicit further questions.
System
History
Cardiovascular:
- Will the patient tolerate surgical stress?
History of hypertension, CAD, previous MI, CHF, valvular diseases, dysrhythmias, implantable cardiac devices (ICDs).
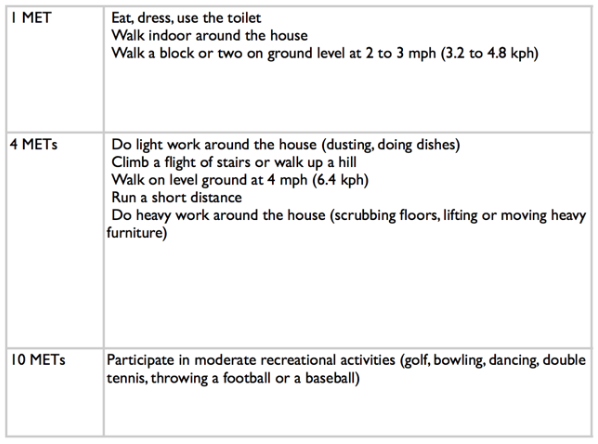
Exercise capacity or metabolic equivalents (METS) – see Figure 1.
Respiratory:
- Will there be issues with oxygenation and ventilation?
Recent upper respiratory tract infection? Smoker?
History of asthma, COPD, OSA?
Dyspnea, wheezing, home oxygen?
STOP BANG score – see Figure 2 (Respiratory Comorbidities).
GI:
- Is this patient at increased risk of aspiration? Does this patient have liver disease and sequelae like coagulopathy?
Increased risk of aspiration
- GERD, inadequate fasting.
- Increased intra-abdominal pressure – obesity, ascites, pregnancy.
- Altered GI motility – diabetes, medications (ex narcotics), bowel obstruction.
Alcohol intake? History of liver disease or infections?
Renal:
- Will there be issues with electrolyte and fluid balance? How will renally cleared medications be affected?
Cause of renal disease.
Dialysis dependent? Schedule for dialysis? Last dialysis session?
- Access for dialysis?
Endocrine:
- Well controlled? Any sequelae from their disease?
Diabetes? Thyroid issues.
Control? Sequelae?
Recent steroid use – reason, dose, duration?
Neurologic and neuromuscular:
- Will neuromuscular blockade be affected? Do I need to have different hemodynamic goals?
History of previous TIAs or strokes? Any current neurological deficits?
Any symptoms of increased intracranial pressure (ex headache, vision changes, nausea, vomiting)?
Spinal cord injuries?
Specific diseases such as myasthenia gravis, multiple sclerosis, or muscular dystrophy?
Figure 1 – Evaluation of Functional Status Using METS (Metabolic Equivalents)
Medications and allergies should be noted.
Past Anesthetic History
Ask about previous anesthetics and any personal or family history of anethestic-related complications, such as malignant hyperthermia, difficult intubation or ventilation, or postoperative nausea and vomiting.
Physical Exam
The physical exam is mainly focused on the airway, cardiovascular, and respiratory systems. Always document a set of baseline vital signs.
Airway:
- Examine general dentition and document any abnormalities such as chipped, loose, or missing teeth.
- Markers of difficult bag mask ventilation using acronym OBESE:
- Obese
- Bearded
- Elderly (> 55)
- Snorer
- Edentulous
- Difficult BMV occurs in 5% of patients.
- Markers of difficult intubation:
- Mouth opening (< 3 fingers may result in difficult or awkward insertion of laryngoscope)
- Mallampati score
- Thyromental distance
- Jaw subluxation
- Reduced neck mobility
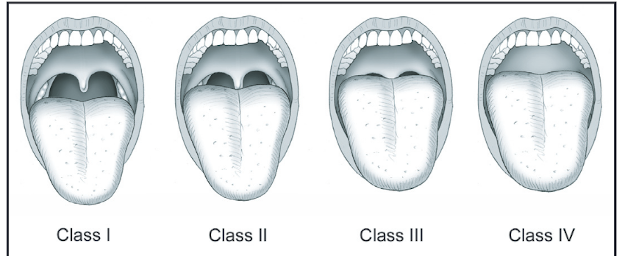
Note: Placeholder image for Malampati score. Replace images with image from Toronto anesthetic record.
Cardiovascular and respiratory examinations should be conducted as usual. If you find any pertinent positives on history, perform the relevant physical exam (for example, a neurological exam for any history of neurological deficits).
Investigations
Commonly ordered investigations include CBC, electrolytes, creatinine, coagulation studies. ECGs and CXRs are no longer recommended for routine screening. However, for patients with pertinent findings on history, ECGs and CXRs may be considered. A pregnancy test may be considered if the woman is of childbearing age and unsure of pregnancy status.
Next page: Preoperative Optimization
Previous page: Overview
