Preoperative Assessment: Respiratory Comorbidities
Obstructive Lung Disease
Asthma
Preoperative:
- Continue bronchodilators on the day of surgery.
- Provide salbutamol prior to anesthesia if patient has active symptoms (e.g. dyspnea/wheeze).
Intraoperative:
- Consider using local / regional anesthesia (e.g. spinal, nerve block) when appropriate.
- If general anesthesia is required, preferentially use less invasive airway manipulations (laryngeal mask airway or mask anesthesia) over endotracheal intubation when appropriate.
- Avoid medications that may release histamine and trigger bronchospasm (e.g. morphine, atracurium, rapid injection of vancomycin).
- Preferentially use agents that promote bronchodilation (propofol, ketamine, sevoflurane, intravenous lidocaine).
- If airway instrumentation is required, it should be performed at deep levels of anesthesia to decrease airway reflexes.
- During mechanical ventilation, set ventilator parameters to allow enough expiration time.
- Treatment options for acute bronchospasm: short-acting inhaled β2 agonists and anticholinergics, glucocorticoids, inhalational anesthetics, ketamine, magnesium, supportive therapy with oxygen and mechanical ventilation.
Postoperative:
- Consider extubation in deep planes of anesthesia (“deep extubation”).
COPD
Preoperative:
- Optimize control and continue puffers.
- Smoking cessation.
- Delay OR for 6 wks after acute respiratory infection.
Intraoperative:
- Consider using local / regional anesthesia (e.g. spinal, nerve block) when appropriate.
- If positive-pressure ventilation is required, be aware of expiratory airflow limitation and risks of breath stacking/dynamic hyperinflation and bullae rupture/pneumothorax.
- Opt for a lung-protective ventilation strategy (6ml/kg) with permissive hypercapnia and allow sufficient expiratory time (avoid high tidal volume, increase expiratory time).
- Avoid targeting lower than baseline PaCO2 in chronic CO2 retainers.
- Treat bronchospasm as previously described (see Asthma section).
- Titrate short or intermediate acting neuromuscular blockers judiciously, ensure complete reversal of neuromuscular blockade at the end of surgery.
Postoperative:
- Carefully titrate supplemental O2 to reach baseline oxygen saturation.
- Optimize pain control while minimizing opioids and sedatives (favour acetaminophen, non-steroidal anti-inflammatories, epidural analgesia, nerve blocks).
- Consider higher levels of postoperative monitoring (intensive care or step-down units, serial arterial blood gas analysis).
Perioperative Management of Obstructive Sleep Apnea (OSA)
See Figure 2 for STOP BANG Score for OSA screening.
Preoperative
- Review sleep study or screen patient for OSA.
- Screen and investigate for OSA-related comorbidities and adequacy of treatment.
- Evaluate and plan airway management options.
- Consider delaying elective surgery for evaluation and initiation of treatment, especially if evidence of obesity hypoventilation syndrome or pulmonary hypertension.
- Determine safety of outpatient surgery.
Intraoperative
- Consider using local / regional anesthesia (e.g. spinal, nerve block) when appropriate.
- During moderate or deeper sedation, maintain high index of suspicion for airway obstruction and use continuous capnography monitoring.
- Minimize use of respiratory depressants: favour shorter-acting anesthetic agents and opioids, ensure complete reversal of neuromuscular blockade at the end of surgery.
- Extubate awake, in head-up position.
Intraoperative
- Carefully monitor in the PACU for adverse respiratory events (desaturations, bradypnea, apnea) and pain-sedation mismatch that may warrant prolonged monitoring.
- Resume CPAP therapy during all moments of sleep, including in the PACU.
- Consider initiating CPAP therapy in patients not previously receiving it.
- Titrate supplemental oxygen to avoid hypoxemia.
- Optimize pain control while minimizing opioids and sedatives (favour acetaminophen, non-steroidal anti-inflammatories, epidural analgesia, nerve blocks).
- Assess adequacy of discharge to unmonitored setting, taking into account underlying risk and adverse respiratory events in PACU.
- Instruct discharged patients to rigorously use CPAP during all periods of sleep until no longer taking opioids.
Figure 2 – STOP BANG Score
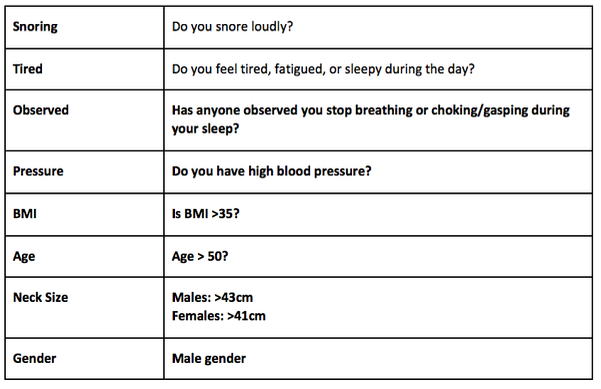
For the general population, OSA risk:
- Low: Yes to 0 - 2 questions
- Intermediate: Yes to 3 - 4 questions
- High: Yes to 5 - 8 questions
- or Yes to 2 or more of the 4 STOP questions + male gender
- or Yes to 2 or more of the 4 STOP questions + BMI > 35kg/m2
- or Yes to 2 or more of the 4 STOP questions + neck circumference 17 inches / 43 in males or 16 inches / 41 cm in females
Previous page: Cardiac Comorbidities
