Preoperative Assessment: Optimization:
Risk Stratification
The Lee Revised Cardiac Risk Index (RCRI) predicts major adverse cardiac events (MACE) in patients with stable ischemic heart disease. These six predictors are:
- High-risk surgery (suprainguinal vascular, intraperitoneal, intrathoracic surgery)
- History of coronary heart disease
- Congestive heart failure
- Diabetes mellitus (type I or type II requiring insulin use)
- Renal insufficiency (creatinine > 175mmol/L)
- Cerebrovascular disease
Patients with 3 or more risk factors have elevated risk of MACE.
Perioperative Medication Management
Cardiovascular medications – in general, most cardiac medications should be continued up to and including the day of surgery, with the exception of ACEi, ARBs, and diuretics. Continuation of antiplatelet and anticoagulation medications (e.g., aspirin, clopidegrel, and DVT prophylaxis agents) depends on the risk of surgical bleeding versus the risk of thrombotic events, especially in patients who have cardiac stents. This is typically a case-based decision and must take into account the reason the medication is needed and the type of surgery being performed.
- Discontinue ACEi, ARB, diuretics
- Continuation of antiplatelets or anticoagulants requires weighing risk of bleeding with risk of thrombotic events
Respiratory medications:
- Puffers should be continued as usual prior to a surgery.
GI:
- Medications aimed at reducing symptoms of reflux should be continued.
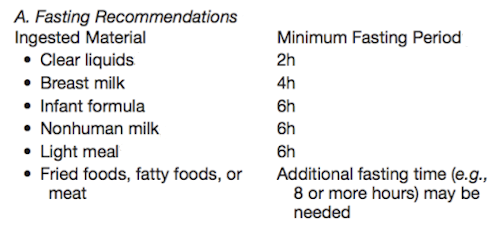
Fasting
The American Society of Anesthesiologists’ Practice Guidelines for fasting prior to elective surgery is as follows:
Postoperative Pain Plan
Depending on the type of surgery, an epidural or nerve block placed before the surgery can be used both intraoperatively as well as postoperatively for pain control. Some patients may benefit from postoperative IV patient controlled analgesia (PCA).
Disposition
Depending on the patient’s preoperative health status as well as the extent and type of surgery, a patient may require a step-down or ICU bed postoperatively for closer monitoring. Patients with sleep apnea may need additional monitoring postoperatively, especially if they are not compliant with CPAP therapy. Patients who remain intubated at the end of a surgery require ICU admission.
Next page: Cardiac Comorbidities
Previous page: Preoperative Assessment
